Perfecting one’s skills in neurological examinations is akin to an artist honing their craft. Among the many techniques requiring mastery, measuring pupil size in a neuro exam is critical. Often a window into the brain’s functionality, pupil measurement allows clinicians to detect subtle changes that may signify neurological issues.
This blog post aims to delve into the comprehensive evaluation of pupil health. In this ever-evolving field, continuous learning and skill refinement are fundamental. After all, in the hands of an adept practitioner, the unassuming act of assessing a patient’s pupils can be a powerful diagnostic tool.
The Three Cardinal Signs of Pupil Measurement
Fundamental to the process of pupil measurement are the three cardinal signs: size, shape, and reaction to light. Each parameter presents a piece of the neurological puzzle. Typically between 2 and 5mm in a normal state, size can alter dramatically in response to conditions such as increased intracranial pressure or Horner’s syndrome. The round shape can be distorted due to trauma or syphilis.
Reaction to light, usually prompt and simultaneous in both eyes, can be sluggish or absent in conditions such as optic neuritis or severe systemic diseases. It’s vital to remember that changes in these signs might be the first indicator of potential neurological issues, underscoring the importance of precise and meticulous assessment.
Essential Tools for Pupil Measurement
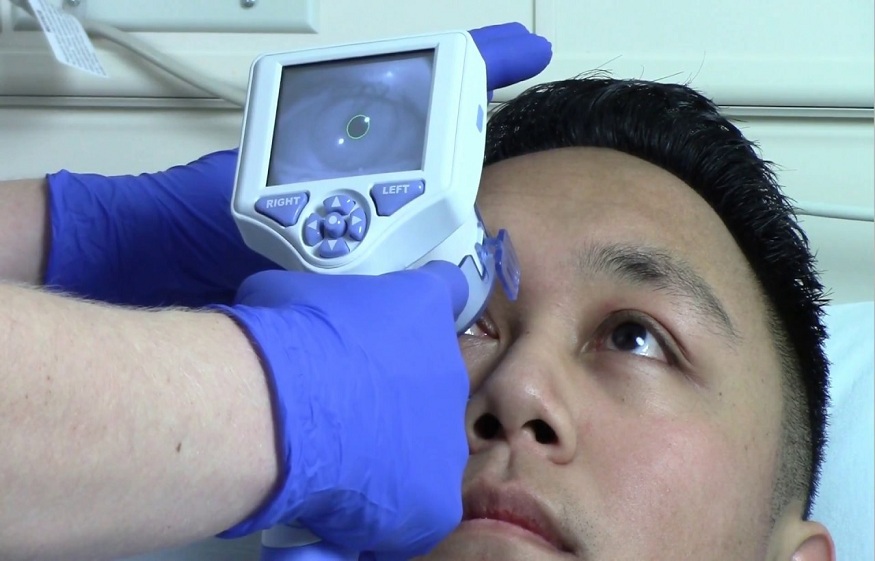
The accuracy of pupil measurement largely hinges on the right set of tools. The humble penlight, a staple in every clinician’s pocket, is a primary tool for evaluating pupil size and light reactivity. While more sophisticated, the pupillometer provides quantitative measurements, reducing inter-examiner variability and improving assessment accuracy.
A slit lamp, though not routinely used for pupil assessment, can provide a magnified view of the pupils, aiding in detecting subtle abnormalities. Choosing the right tool depends on the clinical context; a quick screening might necessitate a penlight, while a detailed evaluation in a neuro-intensive care unit could warrant a pupillometer.
Standardizing the Examination Environment
The importance of a consistent, distraction-free environment for pupil measurement cannot be overstated. Ambient light must be controlled, allowing enough visibility for assessment without causing excessive pupillary constriction.
Patient positioning is also key; a comfortable, upright position usually works best. Clinicians can achieve more accurate and reliable pupil measurements by ensuring these factors are standardized.
The Art of the Swing Technique
The ‘swing technique’ is instrumental in detecting a Relative Afferent Pupillary Defect (RAPD), an important sign of optic nerve disease. The procedure involves swinging a penlight back and forth between the two eyes while observing the pupillary reaction. A healthy response is a direct and consensual constriction, regardless of which eye is illuminated.
However, with RAPD, the affected eye shows a reduced direct response compared to the consensual response when the light is swung from the healthy eye. Mastering this technique requires practice and a keen eye for subtle changes.
Refining the Direct and Consensual Light Reflex Assessment
Evaluating direct and consensual light reflexes is another crucial component of a comprehensive neuro exam. The direct light reflex tests the integrity of the optic nerve, while the consensual response assesses the efferent pathway to the opposite pupil.
Any discrepancy could signal a pathology, such as an afferent pupillary defect or a third nerve palsy. Precision in conducting these assessments and a thorough understanding of the underlying neural pathways can significantly refine the diagnostic process.
Detecting Relative Afferent Pupillary Defects (RAPD)
RAPD, or Marcus Gunn pupil, is a significant clinical finding suggesting a lesion in the optic nerve or severe retinal disease. Detecting RAPD involves observing pupillary responses to the swing technique, as mentioned earlier.
Remember, even a subtle RAPD may be a red flag for potential neurological issues. However, it’s also vital to differentiate it from physiological anisocoria, a benign condition where the pupils are naturally different sizes.
Conclusion:
In the realm of neuro exams, being able to measure pupil size is an essential skill. Mastering the techniques discussed—from evaluating cardinal signs and utilizing tools like the NPi pupilometer effectively to fine-tuning your assessments—can significantly improve the accuracy of your exams.
But remember, as with any skill, perfection comes with practice and a commitment to continuous learning. As you enhance your expertise in this critical aspect of neurology, you’ll find a sense of fulfillment that stems from your ability to provide better patient care.